Translational Research for New Vaccines, Diagnostics, and Treatments
Deep sequencing for culture-free diagnosis of drug resistance in mycobacteria (Deeplex Myc-TB and Deeplex Myc-Lep)
Only 40% of the estimated ~400,000 new tuberculosis cases with rifampicin resistance or multidrug-resistance occurring each year are diagnosed and treated, reflecting major limitations of conventional phenotypic and molecular tests. By building on the progress of next-generation sequencing (NGS) technologies and the knowledge gained on the M. tuberculosis resistome, novel tools for rapid NGS-based, culture-free diagnostics are developed by GenoScreen (Lille) with our collaboration. This led to the development of the first commercial targeted NGS kit for prediction of susceptibility or resistance to 13 anti-tuberculosis drug classes, directly applicable on clinical samples, named Deeplex® Myc-TB. Based on results showing its high degree of accuracy, including in diagnostic trials conducted in Africa, Eastern Europe and Asia (DIAMA H2020 EDCTP; Seq&Treat UNITAID), this novel diagnostic has been endorsed by the WHO in 2023, and is used in >50 countries. We also used this assay to discover ancestral clades of tuberculosis bacilli in East Africa, supporting the East African origin of the pathogen (see Genomics and transcriptomics). We developed a similar first-of-its-kind NGS-based assay for culture-free diagnosis of the agent of leprosy, M. leprae, which is unculturable in vitro. We thereby performed the first nationwide NGS-based survey of leprosy drug resistance in the Comoros, revealing full susceptibility to anti-leprosy antibiotics of M. leprae strains in this country highly affected by this disease.
ERA4TB – European Regimen Accelerator for Tuberculosis – https://era4tb.org/
ERA4TB is a large public–private research consortium launched in 2020 to accelerate the discovery of new tuberculosis (TB) treatment regimens. It brings together over 30 partners from academia, industry, and research organisations funded under the Innovative Medicines Initiative (IMI). The project’s core scientific goal is to build an open, adaptive platform that integrates experimental data, modelling, and simulation to speed up regimen selection and development. ERA4TB uses a parallelised pipeline allowing multiple drug candidates and combinations to be evaluated simultaneously, reducing development time. Key tools include advanced pharmacokinetic–pharmacodynamic modelling, artificial intelligence, and integrated data systems. The platform aims to leverage both new and existing data to inform decision-making and trial design. ERA4TB also engages regulators and stakeholders to support translation. By project end, it aims to deliver at least two new combination regimens ready for Phase II trials and a sustainable platform for future TB drug research. The initiative supports global TB elimination goals by innovating the regimen development process.
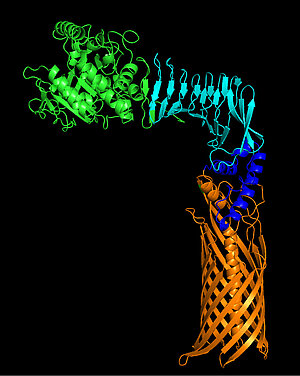
MARVEL : Mechanisms of Activation and Regulation of VirS : Environment- and Ligand-mediated control
Tuberculosis remains a major cause of global mortality, exacerbated by the emergence of multidrug-resistant strains of Mycobacterium tuberculosis. Ethionamide, an antitubercular prodrug, requires enzymatic activation involving at least two proteins, EthA and MymA. Expression of the mymA operon is controlled by the transcriptional regulator VirS.
Alpibectir, the first drug targeting a bacterial transcriptional regulator, interacts with VirS and induces overexpression of the mymA operon. This activation results in both enhanced enzymatic activation of ethionamide and a bacterial physiological imbalance, contributing to Alpibectir’s antibacterial activity.
Because the molecular mechanisms underlying this interaction remain poorly understood, the MARVEL project aims to elucidate the function of VirS, which is thought to act, depending on its state and concentration, as either a repressor or an activator of the mymA operon. A multidisciplinary approach combining biochemistry, biophysics, cryo-EM, and genetics will be employed to characterize its DNA-binding properties, structural organization, environmental signals modulating its activity, and its impact on mycobacterial physiology. The expected outcomes should provide deeper insight into the molecular mode of action of Alpibectir and its global effects on bacterial physiology.
Coordination :
CIIL – RMB - Centre d’Infection et d’Immunité de Lille
Partners :
ULB - Unité Microbiology, Bioorganic and Macromolecular Chemistry Université libre de Bruxelles
SOLEIL - Ligne de lumière PROXIMA-2A Synchrotron SOLEIL
MUSTART : Multiparametric Strategies against Antibiotic Resistance in Tuberculosis
Mustart brings together eight French teams to develop new antibiotics against Mycobacterium tuberculosis, with the goal of shortening and improving the effectiveness of current treatments, which are overly long and promote pharmacological resistance. The consortium explores innovative approaches, including “boosters” capable of restoring the activity of existing drugs and bypassing resistance mechanisms. New chemical libraries expand the chemical space to identify future drug candidates. Several projects target dormant bacilli responsible for relapse, as well as toxin–antitoxin systems involved in bacterial virulence. Other efforts focus on MtPMT as a novel therapeutic target. Mustart also pursues pharmaco-complementary strategies that combine synergistic molecules. This dynamic relies on an integrated pipeline spanning fundamental research to preclinical studies, supported by advanced tools in biophysics, genetics, and animal models. The collective approach and sharing of resources open new therapeutic perspectives against a major global public health challenge.
Coordination :
CIIL – Centre d’Infection et d’Immunité de Lille
Partners :
U1177 – Drugs & Molecules for Living Systems
IPBS – Institut de Pharmacologie et de Biologie Structurale
IP – Institut Pasteur
LMGM – Laboratoire de Microbiologie et de Génétique Moléculaire
SU – Sorbonne Université
TBI – Toulouse Biotechnology Institute
CIRI-HCL – Centre International de Recherche en Infectiologie, Hospices Civils de Lyon
ANR JCJC CycloTub (2023-2027). PI A Machelart
The ANR JCJC CycloTub project aims to improve tuberculosis treatment by using cyclodextrin-based nanoparticles to deliver incorporated antibiotics directly to the lungs. The project is based on the key observation of an intrinsic antibacterial effect that modulates the pulmonary environment, making it less favorable for infection. Within this project, we are investigating the underlying molecular and cellular mechanisms driving this phenomenon.
ANRS-MIE E-NanoTub (2024-2027). PI A Machelart
In the ANRS-MIE E-NanoTub project, we are developing a nanoparticle platform incorporating a combination of antibiotics to treat tuberculosis via aerosol delivery. This project is carried out in collaboration with Ruxandra Gref’s team at the Institute of Molecular Sciences in Orsay. The main objective is to develop hybrid nanoparticles composed of materials with remarkable biological properties, incorporating an optimized combination of antibiotics to deliver treatments locally with the aim of reducing treatment duration, side effects, and environmental contamination.
CPER Resistomics MyCyclo (2024-2026). PI A Machelart
In the MyCyclo project, we are developing nanoparticles to improve tuberculosis treatment. We are particularly interested in the remarkable property of these nanovectors: their preferential accumulation in infected cells. The project aims to understand why these nanoparticles accumulate more in infected cells compared to non-infected cells, as well as to evaluate the potential of these nanovectors when delivered via the pulmonary route. In addition, we are studying the pharmacokinetics of antibiotics incorporated into these nanocarriers to optimize their delivery and local efficacy.
NAVIX - France Vaccins (2026-2029). PI A Machelart
In the Navix project, we are involved in a work package aimed at exploring the advantages of nanocarriers in the development of nasal vaccines. These nanocarriers offer several potential benefits: some possess intrinsic adjuvant properties, while others can enhance the targeting, availability, and half-life of adjuvants or antigens in the nasal epithelium. The goal is to better understand how these nanocarriers can optimize both local and systemic immune responses, contributing to the development of more effective and long-lasting nasal vaccines.
Fondation ULille (2025-2026). PI A Machelart
In this project, funded by the Fondation Université de Lille and co-led by Valentin Sencio, we are exploring the potential of locally administering a recombinant vaccine strain to combat acute respiratory infections. The aim is to assess the efficacy and safety of this local vaccination approach to enhance protection against respiratory pathogens.
FHU Respire – CiblE (2025-2026). PI A Machelart
In the CiblE project, co-led by Valentin Sencio, we are investigating the molecular and cellular mechanisms involved in heterologous protection induced by the local administration of BCG against acute respiratory infections. The goal is to better understand how locally delivered BCG can stimulate protective immune responses against various respiratory pathogens.
B. pertussis SphB1-based secretion platform
In collaboration with ILiAD technology and other researchers in the lab, we are trying to understand the immune response raised by the BPZE1 vaccine strain against both BP and heterologous diseases, which are mainly mediated by inflammation, such as asthma and flu. We are also working to improve the BPZE1 vaccine's expression of heterologous antigens via the SphB1-based secretion platform, with the aim of mediating antigen production and secretion to provide heterologous protection in the context of SARS-CoV2 and M. tuberculosis.
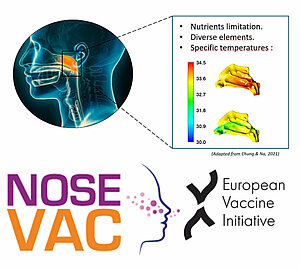
Innovative nasal vaccines to prevent pathogen colonization and infection in the upper respiratory tract - NOSEVAC
We are participating in the European NoseVac consortium, which brings together 11 teams in Europe to develop nasal vaccines to protect against Bordetella infections. We thus characterize host-pathogen adaptation to understand changes in the bacterial and eukaryotic transcriptomes and proteomes during infection, particularly during the initial stages of colonization in the nasal cavity where temperatures are between 32 and 35°C and presenting various concentration of nutriment i.e. transition metal concentrations.